UROTHELIUM
The urothelium that protects the proximal urethra, urinary bladder, and upper urinary tract is where urothelial carcinomas (UC) develop. UC coming from various areas are frequently handled and researched in the same way in daily life and therapeutic trials.
The following are typical bladder symptoms:- urine with blood in it.
- The first sign of bladder cancer is frequently blood.
- Depending on how much blood is present, the color of the urine might range from pink to deep red.
- alteration in urine habits This can involve urinating more frequently than usual.
- a lower back aches.
CAUSES - using tobacco products. taking the diabetes drug pioglitazone (Actos). Smoking, increasing age, Being male, Exposure to certain chemicals, Previous cancer treatment, Chronic bladder inflammation, Personal or family history of cancer.
PREVENTION - Avoid smoking. About half of all bladder malignancies are estimated to be brought on by smoking. Reduce workplace exposure to specific substances. Worker risk for bladder cancer is increased in companies that employ specific organic compounds. Consume a lot of fruits and vegetables along with plenty of water.
TREATMENT - Patients with locally advanced or metastatic urothelial cancers that are inoperable typically receive systemic chemotherapy as their initial treatment. Although multiagent chemotherapy has significant initial response rates, the median survival time is only about 15 months.
URINARY INCONTINENCE
Urinary incontinence, or the inability to control one's bladder, is a frequent and frequently embarrassing issue. The intensity can range from occasionally dribbling pee when you cough or sneeze to having a sudden, intense urge to urinate that prevents you from reaching a restroom in time.
The following are its symptoms: - urine leaks while lifting, bending, coughing, or exercising, among other commonplace duties.
- being unable to hold in urine and experiencing a sudden, intense urge to urinate.
- One may urinate at any time, without reason or notice.
- not having enough time to use the restroom.
CAUSES - Numerous conditions, such as urinary tract infections, vaginal infections or irritations, or constipation, can cause incontinence. Some drugs have the potential to induce momentary bladder control issues. Weak pelvic floor muscles or a weak bladder may be to blame for incontinence that lasts longer.
PREVENTION - keep a healthy weight. Exercise your pelvic floor. Steer clear of bladder irritants like alcohol, coffee, and acidic meals. Consume extra fiber to avoid constipation, which can lead to urine incontinence. If you smoke, give up, or get help to stop.
TREATMENT - Anticholinergics. These drugs may help with urge incontinence and can soothe an overactive bladder. Examples include trospium chloride, tolterodine (Detrol), oxybutynin (Ditropan XL), fesoterodine (Toviaz), darifenacin (Enablex), and tolterodine.
INTERSTITIAL CYSTITIS
Interstitial cystitis is a persistent illness that can cause pelvic pain, bladder pain, and pressure in the bladder. Mild discomfort to severe agony is all possible levels of pain. The ailment is a member of the painful bladder syndrome group of illnesses.
The following are its symptoms: - BPS (interstitial cystitisprimary )'s signs and symptoms include:significant pelvic discomfort (felt over your lower tummy)
- sudden, powerful impulses to urinate
- having an increased need to urinate.
- Lower abdominal discomfort that occurs as your bladder fills and is eased by urinating.
- To go potty, awoke numerous times through the night.
CAUSES - bladder lining injury may make it such that urinating can irritate the bladder and nearby nerves an issue with the pelvic floor muscles that regulate urination. An inflammatory response is being brought on by your immune system.
PREVENTION - You should stay away from comparable items including tomatoes, pickled foods, alcohol, and spices. Some people's symptoms may be made worse by artificial sweeteners. Try removing certain foods from your diet if you suspect they might irritate your bladder.
TREATMENT - Non-steroidal anti-inflammatory medicines (NSAIDs), such as naproxen sodium (Aleve) or ibuprofen (Advil, Motrin IB, among others), are used to treat pain. Tricyclic antidepressants can ease pain and help your bladder relax, such as amitriptyline or imipramine (Tofranil).
KIDNEY STONES
When your urine contains high concentrations of particular minerals, kidney stones, which resemble hard, pebble-like chunks of material, can develop in one or both of your kidneys. If they are treated properly by a medical specialist, kidney stones seldom result in permanent harm. The size and shape of kidney stones might vary.
The following are its symptoms:
- severe, acute discomfort below the ribcage in the side and back.
- groin and lower abdominal pain that spreads.
- wave-like pain with varying levels of severity.
- When urinating, there may be pain or burning.
CAUSES - Possible contributing factors include inadequate hydration, excessive or insufficient activity, obesity, weight loss surgery, and a diet high in salt or sugar. For certain people, family history and infections may be significant. Consuming excessive amounts of fructose is associated with a higher risk of kidney stone formation.
PREVENTION - Making sure you have enough water each day to stay hydrated is the greatest approach to avoid kidney stones. Drink water, but tea and coffee are also acceptable substitutes. Juice some lemons and add it to your water. Keep sodas to a minimum. Eat moderate amounts of salt.
TREATMENT - consuming water Drinking up to 2 to 3 quarts (1.8 to 3.6 liters) of liquid each day can keep your urine diluted and help to ward off the development of kidney stones. Drugs that reduce pain. Small stones might be uncomfortable to pass. Medical treatment to aid with the passage of your kidney stone, your doctor might prescribe a drug.
KIDNEY FAILURE
When your kidneys stop functioning adequately for you to survive without dialysis or a kidney transplant, you have kidney failure. Your kidneys can no longer remove waste from your blood through filtration. End-stage kidney disease (ESKD), sometimes known as end-stage renal disease, is another name for kidney failure (ESRD).
The following are its symptoms:
- decreased urine production, despite the fact that it can occasionally be normal.
- Your feet, ankles, and legs may enlarge as a result of fluid retention.
- respiration difficulty.
- Fatigue.
- Confusion.
- Nausea.
- Weakness.
- abnormal heartbeat
CAUSES - The two most frequent causes of kidney failure are high blood pressure and diabetes. They may also suffer harm as a result of illnesses, diseases, or other ailments.
PREVENTION - A healthy, balanced diet helps lower your risk of kidney disease by maintaining appropriate levels of blood pressure and cholesterol. At least five servings of fruit and vegetables each day should be part of a balanced diet. meals that contain carbohydrates like potatoes, whole-grain bread, rice, or pasta.
TREATMENT - The two treatments for renal failure are dialysis and kidney transplant. In order to remove wastes and extra fluid from your body, dialysis treatments or transplanted kidneys will partially replace the function of your damaged kidneys. Numerous symptoms of yours will improve as a result.
NEPHROGENIC SYSTEM FIBROSIS
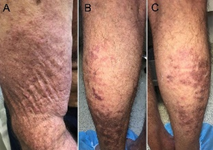
Nephrogenic systemic fibrosis is a rare disease that occurs mainly in
people with advanced kidney failure with or without dialysis. Nephrogenic
systemic fibrosis may resemble skin diseases, such as scleroderma and
scleromyxedema, with thickening and darkening developing on large areas of the
skin.
The
following are its symptoms:
- Swelling
and tightening of the skin
- Reddened
or darkened patches on the skin
- Thickening
and hardening of the skin, typically on the arms and legs and sometimes on the
body, but almost never on the face or head
- Skin
that may feel "woody" and develop an orange-peel appearance
- Burning,
itching or severe sharp pains in areas of involvement
- Skin
thickening that inhibits movement, resulting in loss of joint flexibility
- Rarely,
blisters or ulcers
CAUSES - The exact cause of
nephrogenic systemic fibrosis isn't fully understood. Fibrous connective tissue
forms in the skin and connective tissues, resulting in scarring of tissue
throughout the body, most commonly the skin and subcutaneous tissues. Exposure
to older gadolinium-based contrast agents during MRI has been identified as a
trigger for development of this disease in people with kidney disease. This
increased risk is thought to be related to the kidneys' reduced ability to
remove the contrast agent from the bloodstream. Other conditions may increase
the risk of nephrogenic systemic fibrosis when combined with existing kidney
disease and exposure to older gadolinium-based contrast agents (group 1), but
the link is uncertain. These include Use of high-dose erythropoietin (EPO), a
hormone that promotes the production of red blood cells, often used to treat
anemia, Recent vascular surgery, Blood-clotting problems, Severe infection
PREVENTION - Avoidance of older
gadolinium-based contrast agents (group 1) is key to preventing nephrogenic
systemic fibrosis, as newer gadolinium-based contrast agents (group 2) are
safer and are not associated with increased risk.
TREATMENT - here is no cure for
nephrogenic systemic fibrosis, and no treatment is consistently successful in
halting or reversing the progression of the disease. But patients can consider
the following:
- Hemodialysis.
- Physical
therapy
- Kidney
transplant
- Extracorporeal
photopheresis with ultraviolet A.
https://www.mayoclinic.org/diseases-conditions/nephrogenic-systemic-fibrosis/symptoms-causes/syc-20352299#:~:text=Nephrogenic%20systemic%20fibrosis%20is%20a,large%20areas%20of%20the%20skin.
NEPHROBLASTOMA (WILM’S TUMOR)
Also called Wilm’s Tumor. most common cancer of the kidneys
in children. Wilms' tumor most often affects children ages 3 to 4 and becomes much
less common after age 5.The
following are its symptoms:
Signs and symptoms of Wilms' tumor
vary widely, and some children don't show any obvious signs. But most children
with Wilms' tumor experience one or more of these signs and symptoms:
- An
abdominal mass you can feel
- Abdominal
swelling
- Abdominal
pain
- Other
signs and symptoms may include:
- Fever
- Blood
in the urine
- Nausea
or vomiting or both
- Constipation
- Loss
of appetite
- Shortness
of breath
- High
blood pressure
- Removing
part of the affected kidney.
CAUSES - It's not clear what causes Wilms' tumor, but in rare cases, heredity may play a role. Cancer begins when cells develop errors in their DNA. The errors allow the cells to grow and divide uncontrollably and to go on living when other cells would die. The accumulating cells form a tumor. In Wilms' tumor, this process occurs in the kidney cells. In rare cases, the errors in DNA that lead to Wilms' tumor are passed from a parent to the child. In most cases, there is no known connection between parents and children that may lead to cancer.PREVENTION
- Wilms' tumor can't be prevented by anything you or your child can do. If your
child has risk factors for Wilms' tumor (such as known associated syndromes),
the doctor may recommend periodic kidney ultrasounds to look for kidney
abnormalities. Although this screening can't prevent Wilms' tumor, it may help
detect the disease at an early stage.
TREATMENT
- treatment for Wilms' tumor usually
involves
- Surgery and chemotherapy,
- Sometimes radiation therapy.
- Surgery to remove all or part of a kidney.
- Removing
the affected kidney and surrounding tissue.
- Removing
all or part of both kidneys.
is a kidney disorder that causes your body to pass too much protein in your urine.
The following are its symptoms:
- puffy eyelids and swelling in the legs, ankles, feet, lower abdomen, or other parts of your body
- foamy urine
- weight gain due to retaining too much fluid
- tiredness
- loss of appetite
CAUSES - Many disorders can cause nephrotic syndrome, including diseases that affect only the kidneys and diseases that affect many parts of the body, such as diabetes and lupus.
PREVENTION - You can't prevent some causes of nephrotic syndrome. But you can take action to avoid damage to your glomeruli: Manage high blood pressure and diabetes, if you have them. Be sure to get vaccines for common infections, especially if you work around people who have hepatitis or other diseases.
TREATMENT - Treatment varies according to symptoms, causes, and the extent of kidney damage. Symptoms of nephrotic syndrome are most often treated with these medicines3
- an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB). ACEs and ARBs can help reduce protein loss and also lower blood pressure, which is often high in people with nephrotic syndrome.
- a diuretic (water pill), which reduces swelling by helping the kidneys remove fluid from the blood.
In some cases, your health care professional may also prescribe medicines that lower cholesterol, called statins NIH external link. Blood thinners NIH external link may also be used, but usually only if you develop a blood clot.
People with nephrotic syndrome should receive the pneumococcal vaccine External link, along with yearly flu shots, to prevent viral and bacterial infections.
https://www.niddk.nih.gov/health-information/kidney-disease/nephrotic-syndrome-adults
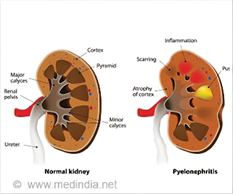
PYELONEPHRITIS
A kidney infection is a type of urinary tract infection (UTI). A kidney infection may begin in the tube that carries urine from the body (urethra) or in the bladder. The infection can travel to one or both kidneys. A kidney infection is also called pyelonephritis.
The following are its symptoms:
- Fever
- Chills
- A burning feeling or pain when urinating
- Having to urinate often
- A strong, lasting urge to urinate
- Back, side or groin pain
- Nausea and vomiting
- Pus or blood in the urine
- Urine that smells bad or is cloudy
- Belly pain
CAUSES - Bacteria that enter the urinary tract through the urethra can multiply and travel to your kidneys. This is the most common cause of kidney infections. Bacteria from an infection in another part of the body also can spread through the bloodstream to the kidneys. In rare cases, an artificial joint or heart valve that becomes infected can cause a kidney infection. Rarely, a kidney infection happens after kidney surgery. PREVENTION - Reduce your risk of kidney infection by taking steps to prevent urinary tract infections. Women in particular may lower the risk of urinary tract infections if they: Drink fluids, especially water. Fluids can help remove bacteria from the body when you urinate. Urinate as soon as you need to. Don't delay urinating when you feel the urge. Empty the bladder after sexual intercourse. Urinating as soon as possible after sex helps clear bacteria from the urethra. This lowers the risk of infection. Wipe carefully. Wipe from front to back after urinating and after a bowel movement. This helps prevent bacteria from spreading to the urethra. Avoid using products in the genital area. Deodorant sprays in the genital area or douches can be irritating.
TREATMENT - oral antibiotic therapy with a fluoroquinolone is successful in most patients with mild uncomplicated pyelonephritis. Other effective alternatives include extended-spectrum penicillin's, amoxicillin-clavulanate potassium, cephalosporins, and trimethoprim-sulfamethoxazole.
https://www.mayoclinic.org/diseases-conditions/kidney-infection/symptoms-causes/syc-20353387#:~:text=A%20kidney%20infection%20is%20a,infection%20needs%20prompt%20medical%20treatment.
URINARY INCONTINENCE
Urinary incontinence means a person leaks urine by accident. While it can happen to anyone, urinary incontinence, also known as overactive bladder, is more common in older people, especially women. Bladder control issues can be embarrassing and cause people to avoid their normal activities
The following are its symptoms:
- Leaking urine when coughing, sneezing, laughing, or exercising
- Feeling sudden, uncontrollable urges to urinate
- Frequent urination
- Waking up many times at night to urinate
- Urinating during sleep
CAUSES - Incontinence can happen for many reasons, including urinary tract infections, vaginal infection or irritation, or constipation. Some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to:
Weak bladder or pelvic floor muscles. Overactive bladder muscles. Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinson’s disease. Diseases such as arthritis that may make it difficult to get to the bathroom in time Pelvic organ prolapse, which is when pelvic organs (such as the bladder, rectum, or uterus) shift out of their normal place into the vagina or anus. When pelvic organs are out of place, the bladder and urethra are not able to work normally, which may cause urine to leak. Most incontinence in men is related to the prostate gland. Male incontinence may be caused by: Prostatitis, a painful inflammation of the prostate gland Injury or damage to nerves or muscles from surgery an enlarged prostate gland, which can lead to benign prostate hyperplasia, a condition in which the prostate grows as men age
PREVENTION - Urinary incontinence isn't always preventable. However, to help decrease your risk:
- Maintain a healthy weight
- Practice pelvic floor exercises
- Avoid bladder irritants, such as caffeine, alcohol and acidic foods
- Eat more fiber, which can prevent constipation, a cause of urinary incontinence
- Don't smoke, or seek help to quit if you're a smoker
TREATMENT - Pelvic floor muscle training, Electrical stimulation, Biofeedback, Bladder training, Incontinence products, Medicine (Antimuscarinics)
https://www.nia.nih.gov/health/urinary-incontinence-older-adults#:~:text=Urinary%20incontinence%20means%20a%20person,to%20avoid%20their%20normal%20activities.
https://www.nhs.uk/conditions/urinary-incontinence/treatment/#:~:text=Incontinence%20products,-While%20incontinence%20products&text=absorbent%20products%2C%20such%20as%20pants,for%20example%2C%20while%20you%20exercise








Comments
Post a Comment